More Information
Submitted: November 30, 2020 | Approved: December 30, 2020 | Published: January 01, 2021
How to cite this article: Chalise HN. Fears of health catastrophe as Nepal reports increasing deaths from COVID-19. Arch Psychiatr Ment Health. 2021; 5: 001-003.
DOI: 10.29328/journal.apmh.1001027
Copyright License: © 2021 Chalise HN. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Coronavirus disease; COVID-19; COVID-19 pandemic; COVID-19 fear
Fears of health catastrophe as Nepal reports increasing deaths from COVID-19
Hom Nath Chalise1-3*
1Faculty Member, Department of Public Health, Nobel College affiliated to Pokhara University, Sinamangal, Kathmandu, Nepal
2Research Coordinator, Jeevan Bikas Samaj, Katahari, Morang, Nepal
3Vice presdent, Population Association of Nepal, Kathmandu, Nepal
*Address for Correspondence: Dr. Hom Nath Chalise, Department of Public Health, Nobel College affiliated to Pokhara University, Sinamangal, Kathmandu, Nepal, Tel: +977 9851012622; Email: [email protected]
Coronavirus disease 2019 (COVID-19) had affected both developed and developing countries too. The first case in Nepal was confirmed on 23 January 2020. It was also the first recorded case of COVID-19 in South Asia. Nepal reported its first COVID-19 death on May 16. At the end of October, the number of death stood 937 and 1126 on 9 November. In September and October, deaths doubled, and with winter setting in, fatalities may skyrocket. Among the total CP cases in Nepal nearly 50% are from the Capital Kathmandu. So, Kathmandy is the new epicenter of COVID-19 in Nepal. There are no proper community-based isolation centres and ICU beds are also still limited. Due to increasing trend of COVID-19 cases and death people have fear of psychological stress. A study shows at least one symptom of psychological distress whereas 32% suffered from two or more symptoms of psychological distress such as restlessness, fearfulness, anxiety and worry and sadness. Despite limited resources, the government’s major challenges are early diagnosis, management of confirmed cases, contact tracing, and implementing some public health measures to reduce the infection’s transmissibility.
Coronavirus disease 2019 (COVID-19), which is widely accepted as having first identified and spread from Wuhan, China, is declared a pandemic by WHO on 11th March 2020 [1]. COVID-19 pandemic (CP) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As of 10th November 2020, there have been more than 50 million confirmed cases CP, with 1.27 million deaths and more than 36 million recovered [2]. The Latest data shows, CP had affected both developed and developing countries too [3,4]. CP started in Nepal about 3 months later than in China. This indicates that nature tried to protect Nepal giving adequate time to learn about the pandemic and to make preparations to face it.
Nepal is one of the world’s poorest and most populous regions. The first case in Nepal was confirmed on 23rd January 2020 when a 31-year-old student, who had returned to Kathmandu from Wuhan on 9 January, tested positive for the disease 9 [1,5]. It was also the first recorded case of COVID-19 in South Asia [3,4]. Nepal’s first case of local transmission was confirmed on 4 April in Kailali District. The first death occurred on 14th May. [6] A country-wide lockdown came into effect on 24th March 2020, and ended on 21st July 2020 [5,6]. As of 9th November 2020, the Ministry of Health and Population (MoHP) has confirmed a total of 197,024 cases, 159,724 recoveries, and 1,126 deaths in the country [6].
Initially, most of the confirmed cases were imported from other countries in Nepal [1,5,6]. Nepal was braced for a “major outbreak” after some thousands of migrants returning from India tested positive for the COVID-19. Initially, the majority of CP cases in Nepal have been either Indian nationals or Nepali workers who have recently returned from India due to open and porous borders between India and Nepal [1,5]. At first, major outbreaks were seen in Eastern area (Udayapur district), Western area (Banke district) and Central area (Birgunj) of Nepal which were directly linked with people coming from India. But, since the beginning of September 2020, Kathmandu (Capital) is considered the epicenter of CP and nearly half of all the COVID-19 cases are reported from Kathmandu alone only. Further, now Nepal ranks in 34th country with 200 thousands reported COVID-19 cases [2].
But the CP death rates are unequal across age groups. Since the CP death rate increases sharply with age, the larger the older population, the greater the challenges for communities and societies. Early data from Nepal shows people most affected from CP were people of young age group both in terms of infection and death [7]. But, the latest data shows that people of higher age groups are more vulnerable to CP like many other countries. Many studies show older adults are more likely than younger people to have pre-existing conditions such as cardiovascular disease, diabetes, chronic respiratory disease, hypertension, and cancer. It makes older people more vulnerable to CP.
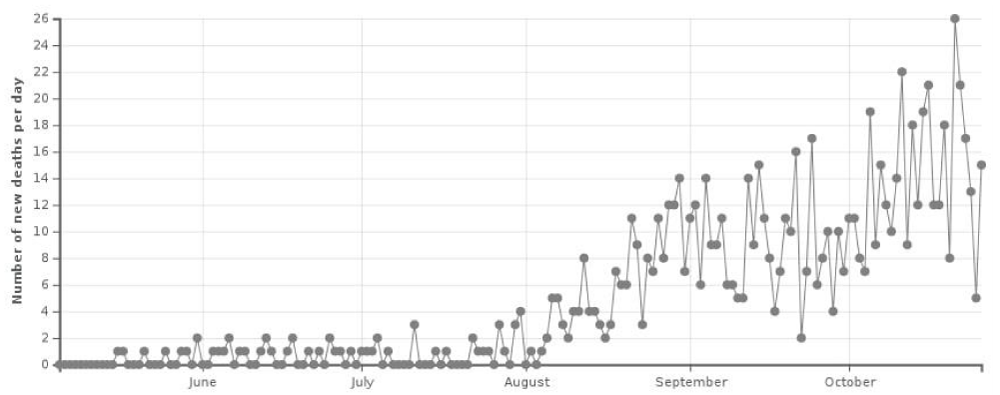
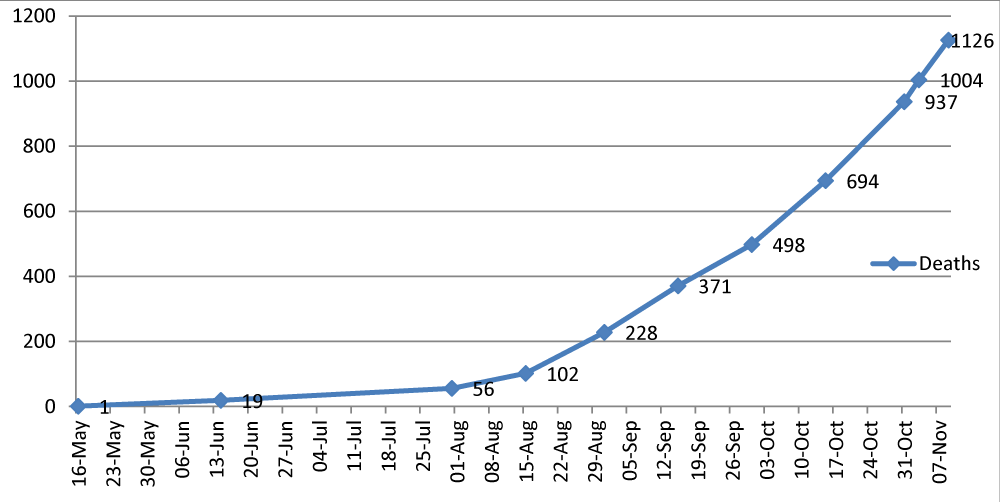
Figure 1 and Figure 2 shows the daily and cumulative CP death chart of Nepal. Nepal reported its first COVID-19 death on May 16th [8]. At the end of August, the number of death stood 228 which went up to 498 at the end of September and 937 at the end of October [6]. In September and October, deaths doubled, and with winter setting in, fatalities may skyrocket. But if the data of Nepal Army, which has been managing the bodies of the people infected with CP for their last rites, is anything to go by, the number of CP deaths has been quite higher than the government reported [9]. Among the total CP cases in Nepal, nearly half of all cases are reported in the capital Kathmandu and its surrounding areas, home to 4 million of the country’s 30 million people. Similarly, more than 50% active cases of CP (total 36174 as of 9th November 2020) are also from Kathmandu. Among 1126 deaths also nearly 40% are from Kathmandu [6]. So, people living in Kathmandu valley are more vulnerable to CP these days.
Figure 1: Daily new deaths from COVID-19 in Nepal.
Figure 2: Total death from COVID-19 in Nepal.
CP has created so many mental and psychological health issues [8,10]. A COVID-19 study from Nepal shows half of the respondents suffered from at least one symptom of psychological distress whereas 32% sufered from two or more symptoms of psychological distress such as restlessness, fearfulness, anxiety and worry and sadness[11]. The outbreak of COVID-19 has raised concerns about the potential for a widespread increase in mental health issues [12]. People could experience fear of death.
With the recent tremendous increase, CP cases along with daily more than 20 deaths have also increased the fear among Nepalese. The sudden interpersonal loss associated with CP, along with severe social disruption, can easily overwhelm the ways individuals and families cope with bereavement [13]. This devastating pandemic has affected nearly every aspect of daily life. The necessary social distancing and quarantine measures implemented as mitigation strategies have significantly amplified emotional turmoil by substantially changing the social fabric by which individuals, families, communities, and nations cope with tragedy. The effect is multidimensional disruption of employment, finances, education, health care, food security, transportation, recreation, cultural and religious practices, and the ability of personal support networks and communities to come together and grieve [13].
One study found the long prevalence of this pandemic has created different types of psychological disorders and chaos among Nepalese people [14]. The psychological issues due to CP death in Nepal may hit in several ways due to considerably low socio-economic status and fragile health care system. Country was in full lockdown more than four months. The government is not prepared to handle the catastrophic situation. There are no proper community-based isolation centres and ICU beds are also still limited. Further, Nepal government controversy statement about the free test and treatment of CP suspected patients, not to visit the hospital unless someone is quite serious and handling the death body has also created some dilemma and fear in Nepalese people. Further the situation that most of the hospital beds in Kathmandu are fully occupied with CP patients and it is not easy to get the beds for general people has also created lots of fear and stress among Nepalese people. Some people are already in stress as they are facing the problem of hands to mouth.
Therefore, the government’s major challenges are early diagnosis, management of confirmed cases, contact tracing, and implementing some public health measures to reduce the infection’s transmissibility. Despite the limited resources, Nepal government is trying its best to cope with CP. As the health care system of Nepal is fragile and lacks the necessary infrastructure to cope with an increasing number of CP, the country is not ready for a full epidemic. Nepal still needs to focus on strengthening the health care system countrywide to control the present and future epidemics. Nepal should also focus on mass counseling to get rid of the psychological fear of CP and other issues resulting from it.
- Chalise HN. COVID-19 Situation and Challenges for Nepal. Asia Pacific Journal of Public Health. 2020; 32: 281–282. PubMed: https://pubmed.ncbi.nlm.nih.gov/32545991/
- Worldometer. COVID-19 coronavirus pandemic, USA, 2020. https://www.worldometers.info/coronavirus/
- Chalise HN. South Asia is more vulnerable to COVID-19 pandemic. Arch Psychiatr Ment Health. 2020; 4: 046-047. https://www.psychiatryhealthjournal.com/fulltext/apmh/apmh-aid1018.php
- Chalise HN, Pathak KP. Situation of COVID-19 Pandemic in South Asia. J Health Allied Sci. 2020; 10: 11-14.
- Chalise HN. COVID-19 situation in Nepal. Arch PsychiatrMent Health. 2020; 4: 033-034. https://www.psychiatryhealthjournal.com/fulltext/apmh/apmh-aid1015.php
- Novel coronavirus (COVID-19) media briefing. Ministry of Health and Population (Nepal). 2020; https://covid19.mohp.gov.np/
- Chalise HN, Rosenberg E. COVID-19 and Immunity in the Elderly. J Geriatric Med. 2020; 02:
- Chalise HN, Dhungana HN. Fears of COVID-19 catastrophe as Nepal reports death from new Coronavirus. J Phys Med Rehabil Disabil. 2020; 6: 047.
- Kathmandu Post. Nepal’s Covid-19 death toll crosses 1,000 mark. 2020. https://tkpo.st/2I4oZlj
- Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, ET AK. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020; 7: 228–229. PubMed: https://pubmed.ncbi.nlm.nih.gov/32032543/
- Gautam K, Adhikari RP, Gupta AS, Shrestha RK, Koirala P, et al. Self-reported psychological distress during the COVID-19 outbreak in Nepal: findings from an online survey. BMC Psychol. 2020; 8: 127. PubMed: https://pubmed.ncbi.nlm.nih.gov/33298196/
- Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020; 66: 317–320. PubMed: https://pubmed.ncbi.nlm.nih.gov/32233719/
- Simon NM, Saxe GN, Marmar CR. Mental Health Disorders Related to COVID-19–Related Deaths. JAMA. 2020; 324: 1493–1494. PubMed: https://pubmed.ncbi.nlm.nih.gov/33044510/
- The Himalayan Times. Psychosocial problems due to COVID-19 and coping mechanisms. https://thehimalayantimes.com/opinion/psychosocial-problems-due-to-covid-19-and-coping-mechanisms/